TEMPORALMANDIBULAR JOINT
Introduction
- Temporomandibular joint or craniomandibular joint is a form of articulation found only in mammals. This is called as Temporomandibular joint because this joint is formed by the articulation of mandibular condyle at the base of the cranium with the squamous part of temporal bone.
- Also known as craniomandibular joint as the mandible is connected to the cranium through this joint. Temporomandibular is by far the most complex joint in the body.
- As it provides hinging movement in one plane forward and backward like hinge of a door it is called as ginglymoid joint. However, at the same time it also provides gliding movement which classifies it as an arthrodial joint so known as ginglymoarthrodial joint.
- It is known as a modified ball socket type of joint as it allows movements in three planes, sagittal, transverse and coronal. It is also known as compound joint. Compound joint is the joint formed by these articulation of three bones. As the articular disc functionally serves as a non-ossified bone that permits the complex movements of the joints, the joint is called even as a compound joint.
- The physiologic activities in which the temporomandibular joint plays a part may be voluntary or reflex and ranges from mastication, deglutition and phonation, to such momentary actions such as grasping and yawning.
Development of Temporomandibular Joint
- The mammalian craniomandibular articulation develops anterolateral to the otic capsule from the first branchial arch mesenchyme and is therefore innervated by fifth cranial nerve. This is the early embryonic joint.
- This primary embryonic joint is formed by the joining or is the joint between malleus and incus which develops from first branchial arch. The malleus and incus are formed by differentiation of large islands of cartilage, found in the middle ear cavity. This joint serves as the primary TMJ joint up to 16 weeks of prenatal life. This joint is an uniaxial hinge joint capable of no lateral motion.
- By the end of 7-11 weeks of gestation the secondary TMJ begins to develop. At about ninth prenatal week a condensation of mesenchyme appears surrounding the upper posterior surface of rudimentary ramus.
- This mass chondrifies at about 10-11 weeks to form cartilaginous mandibular condyle. With progressive endochondral ossification the cartilage fuses with the posterior part of the bony mandibular body. At about 9-10 weeks the muscle fibers become more differentiated Blood vessels, nerves etc. can be seen clearly present in the joint region at about 10 weeks of gestation.
- The appearance of mandibular fossa of the temporal bone is some what earlier than that of the condyle (u) at about 7-8 weeks. Ossification of the fossa is more prominent at about 10-11 weeks. Ossification continuous in this region and at about 22 weeks the mandibular fossa shows both medial and lateral walls and articular eminence is evident. The shape of the fossa is concave at about the ninth week and it takes the definitive concave shape to match the convex condyle. The differentiating mesenchymal cells interposed between the condyle and mandibular fossa gives rise to the capsular and intracapsular structures of the TM joints.
Articular Disc
- Articular disc is first seen at about seven and one half weeks. By the 10th week first signs of collagenous fibers within the articular disc develops and it becomes more pronounced by 12 weeks. From the 19-20th week the disc increasingly takes on its definitive fibro cartilaginous composition. At this stage only the disc shows pattern of differential cell proliferation in which central region becomes thinner than periphery.
Articular Capsule
- The articular capsule first appears at about 9-11 weeks. By the 17th week the capsule is seen as fully formed tissue boundary between intracapsular and extracapsular components of the TMJ. By the 13th week the lower cavity of the fossa enlarges and the superior joint cavity becomes more evident. The shapes of the joint cavities are reciprocal at the time when the upper joint cavity is concave the lower joint cavity is convex.
- Works done by Hooker (1954 and Humphrey (1968) shows that actual mouth opening actions are observable as early as 7-8 weeks of gestation.
- But certain others like Symons (1952), Perry (1985), Moffet (1957) said that only scattered muscle fibers of lateral pterygoid muscle are clearly discernible at 7-8 weeks. Therefore, the prenatal jaw opening activity that both Hooker and Humphrey observed is said to have involved the articulations of the primary TMJ.
Anatomy of the TMJ
- The temporomandibular joint or craniomandibular articulations is the articulation between the lower jaw and the cranium. The bony elements of this joint are the squamous part of the temporal bone above and the mandibular condyles below. This articulation consists of two synovial joints, the left and right temporomandibular joint.
- TMJ is complex both morphologically and functionally. An articular disc composed of dense fibrous tissue is interposed between the temporal bone and the mandible dividing the articular space into an upper and lower compartment, gliding movement occurs in upper compartment and the lower compartment functions as a hinge joint. The articulating surface of the TMJ are lined by dense, avascular fibrous connective tissue.
Relations of TMJ
|
Laterally |
1)
Skin, Fasciae. 2) Parotid gland. 3) Temporal branches of the VII nerve.
|
|
Medially |
Tympanic plate separates TMJ from internal carotid artery, spine of the sphenoid with upper end of Sphenomandibular ligament, Auriculotemporal and chorda tympani. Middle meningeal artery. |
|
Anteriorly |
Lateral
pterygoid muscles. Masseteric nerve and vessels. |
|
Posteriorly |
The parotid gland separates it from external acoustic meatus. |
|
Superiorly |
Middle
cranial fossa Middle meningeal vessels. |
|
Inferiorly |
Maxillary artery and vein |
|
Blood supply |
Superficial temporal artery and maxillary artery |
|
Nerve supply |
Auriculotemporal nerve and masseter nerve. |
FUNCTIONAL ANATOMY OF THE TMJ
Mandibular condyle
- This is convex in shape and it articulates with the articular fossa which is separated into the upper and lower compartments by the articular disc. it present as an ovoid bony knob like process on a narrow mandibular neck. The adult condyle is about 15-20mm mediolaterally and 8-10mms anterioposteriorly. The articular surface of the condyle faces upwards and forwards so that in side view the neck of the condyloid process seems to bend forward. The lateral pole of the condyle extends slightly beyond the ramus and is roughened for the attachment of articular disc and temporomandibular ligament.
Articular disc
- Each human TMJ is essentially a double joint due to the presence of an intra articular disc.
- The articular surface are of fibrous tissue, condylar perichondrium and temporal periosteum. Technically classified as a ginglymoarthrodial joint. It adjusts itself to the changing contours of the condyle head as it moves in the fossa. This is possible as the disc is not uniformly thick, but is modified in different regions. The underside of the disc is concave and fits closely over the condylar head like a cap. This ensures the rotatory movements of the condylar head in the fossa and the disc moves along with the condyle.
- In sagittal section, the disc is divided into three regions according to thickness. The central area is the thinnest and is called intermediated zone. In a normal condyle is located In the intermediate zone of the disc, bordered by thicker anterior and posterior regions. From anterior to posterior the disc shows five zones :
1)
Anterior extension
2)
Anterior band
3)
Intermediate zone
4)
Posterior extension
5) Posterior band
- Posteriorly the disc is bilaminar. The thickened anterior and posterior bands forms an ellipsoidal doughnut. This ellipsoidal doughnut functions to stabilize the condylar head in the glenoid fossa with the jaws at rest. The disc is thus considered as a flexible, viscoelastic adapter which helps the moving joint surface achieve more off effective articular surface congruity.
Articular- fossa
- This is the concavity within the temporal bone that houses the mandibular condyle. The anterior wall of the fossa is formed by articular eminence and posterior wall is formed by the tympanic plate.
- The fossa is lined by articular tissue. The posterior part of the fossa elevated to a ridges called the posterior articular lip.
- The posterior articular lip is higher and thicker at its lateral end and is known as post glenoid process. Medially the articular fossa is bounded by a bony plate that leans against the spine of sphenoid sometimes drawn into a triangular process and is known as the temporal spine.
Articular capsule
- The capsule forms a thin, fibrous connective tissue sleeve about the joint which tapers from above down to the condyle neck. It is attached to squamous temporal bone just peripheral to the margins of the articulating surfaces. They are vertically oriented and are of such a length so as enable the normal range of joint movements. All the non articulating surface within the capsule form synovial membrane, the surface area of which is increased by the formulation of villi and folds. The synovial fluid is a dialysate of plasma with added, mucins and proteins. The cells it contains are mainly lymphoid or macrophage in type. The thickened anterolateral and lateral portions of the capsule which is attached to the articular tubercles is called temporomandibular ligament.
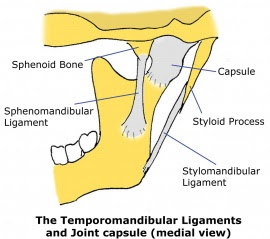
Ligaments of temporomandibular joint
- Ligaments limit the movements of temporomandibular joint. The capsule is too delicate a structure to support the joint unaided and so joint stability is achieved with intrinsic and extrinsic ligaments.
- Intrinsic ligaments (directly involved with movement of joint and attached in relation to joint).
- The main intrinsic ligament is the temporomandibular ligament or the lateral ligament. It is located lateral to the capsule. The fibers of the ligament pass obliquely from its wide origin lateral to the articular tubercle to a narrow insertion in the neck of the condyle, below and behind the lateral pole of the condyle. Collateral ligaments also act as intrinsic ligaments. These are rather narrow bands of collagen fibers that run horizontally backwards on the inner aspect of the capsule from the lateral and medial aspects of the articular eminence to the respective condylar poles. These restrict the distal displacement of condylar head. These collateral ligaments along with the temporomandibular ligaments, helps to attain the clinical ligamentous position.
Extrinsic ligaments
- These are not directly involved with the joint, but they modify the range of movements that are possible.
- These are also known as accessory ligaments and they include -
1)
Sphenomandibular ligament
2)
Stylo mandibular ligament
3)
Pterygomandibular raphe
4)
Temporomandibular ligament
of the opposite
side which acts as an extrinsic
medial ligament.
Sphenomandibular ligament
- Attached superiorly to the spine of the sphenoid and inferiorly it is attached to the lingula of the mandibular foramen. It is a remnant of the cephalic end of Meckel's cartilage.
Stylomandibular ligament
- It is attached above to the lateral surface of styloid process and below to the angle and posterior border of the ramus of the mandible.
- Fibrous capsule and articular disc also serves as the ligaments of TM joint.
REFERENCES
1. Anatomy Of Head And Neck - Chourasia.
2. Applied Physiology Of Mouth - Lave I ie
3. Functional Anatomy Of Oral Tissues - Shaw J. H.
4. The Structure And Function Of Temporomandibular Joint - G. S. Mackay, R. Yemm.





👏🏻
ReplyDeleteThank you
Delete